
Headache and COVID-19: A multifaceted association unveiling the complexity of SARS-CoV-2 infection
The severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) is responsible for coronavirus disease 2019 (COVID-19), a complex condition characterized by severe respiratory impairment and systemic disorders.1 From December 2019—when SARS-CoV-2 was first discovered in Wuhan, China—to February 2022, over 418 million cases of COVID-19 have been confirmed worldwide, including over 5.8 million deaths,2 making it one of the biggest global health concerns of our time. One of the main features of COVID-19 is its complex pathophysiology that involves multiple organs, including the nervous system.3 According to a medical chart review study, more than 90% of patients with a SARS-CoV-2 infection reported subjective neurological symptoms,4 with headache being frequently reported both during the acute and the healing phases.5 After two years from the start of the pandemic, researchers are starting to shed light on the possible links between headache and COVID-19, revealing interesting analogies with the pathophysiology of migraine.6
HEADACHE IS MORE FREQUENT AMONG PEOPLE WITH A HISTORY OF HEADACHE DISORDERS
The prevalence of headache associated with COVID-19 is a debated matter, with studies reporting values ranging from 10 to 70%.6 Despite the high variability of these results, which might be explained by the different design and objectives of research studies,6 headache is consistently described as a frequent symptom of COVID-19.6-8 Indeed, according to several studies, headache is the fifth most frequent general symptom of COVID-19 (after fever, cough, myalgia or fatigue, and dyspnea),9-11 and the fourth most frequent neurological symptom associated with the disease (after gustatory or olfactory dysfunctions, and myalgia) (Figure 1).12 Headache associated with COVID-19 seems to affect more women,6 people of young age6 and those with a history of headache disorders.6,7 However, data have also shown that headache can even manifest in people who have never experienced a headache disorder prior to COVID-19,7,8 thus suggesting that the SARS-CoV-2 infection itself or the subsequent disease might play a causative role in the new onset of this symptom.12
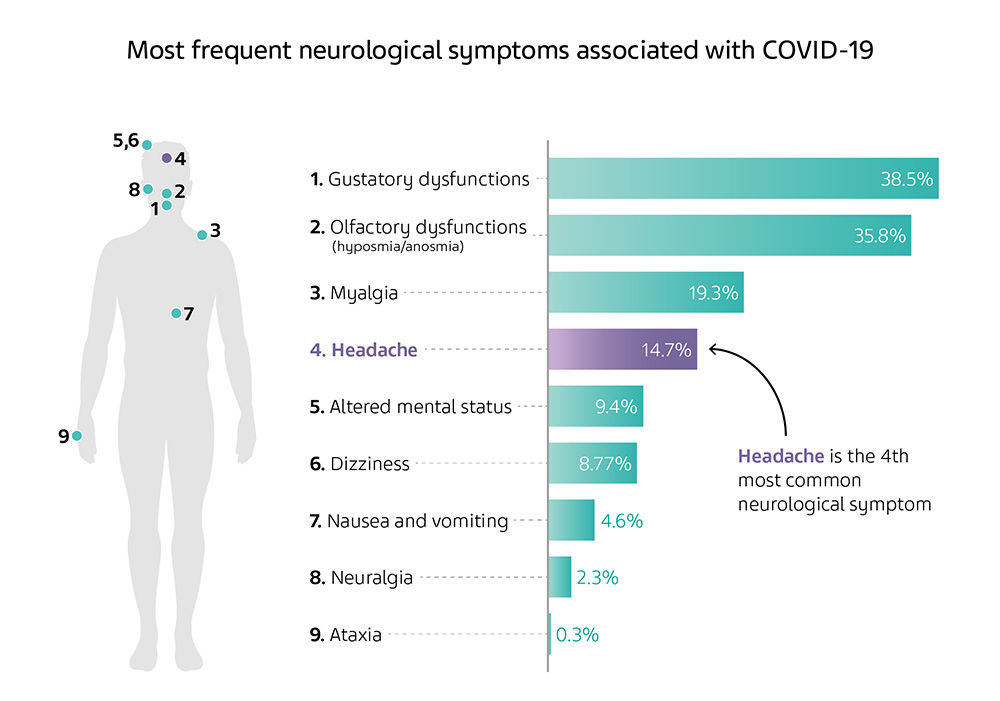
Adapted from Table 1 of Harapan BN, et al. J Neurol 2021;268:3059-71.
Figure 1. Most frequent neurological symptoms associated with COVID-19
HEADACHE ASSOCIATED WITH COVID-19 CAN BE CLASSIFIED INTO THREE PHENOTYPES
Several studies conducted since the COVID-19 outbreak have described the characteristics of headache associated with the disease, highlighting the presence of three main phenotypes: migraine-like, tension-type headache (TTH), and COVID-19-specific headache.1 The migraine-like phenotype associated with COVID-19 mainly affects people with a history of migraine, who also reported, during the infection, higher incidences of nausea, vomiting, photophobia, phonophobia, pulsatile pain and worsening pain following physical activity.1 Instead, individuals reporting TTH related to COVID-19 described a mild to moderate headache, which is pressing and does not worsen with movement.1 COVID-19-specific headache is a new phenotype that has never been described before.1 It is similar to migraine but often lacks some typical migraine features such as photophobia, nausea and vomiting.1 In this phenotype, pain is typically bilateral and mainly localizes in the frontal area of the head.1 It is usually intense and pressing, and its severity may increase after physical activity and head movement.1 Moreover, COVID-19-specific headache can sometimes be accompanied by phonophobia.1 According to a study, among these three headache phenotypes, TTH is the most frequently associated with COVID-19, followed by migraine, which is reported in 25% of cases.6 No data were provided on the prevalence of the COVID-19-specific headache.
Headache phenotype as a possible predictor of COVID-19 prognosis
According to some data, headache phenotypes might be helpful predictors of the viral infection prognosis.13 In one retrospective cross-sectional study, researchers looked for associations between headache features, COVID-19 symptoms and laboratory tests of hospitalized patients with a confirmed diagnosis of COVID-19.13 In the study cohort, migraine-like phenotype was associated with more severe forms of COVID-19, and showed to be often accompanied by multiple biomarkers of COVID-19-related complications—such as thrombocytopenia, lymphopenia and hyperferritinemia, along with increased levels of C-reactive protein (CRP) and procalcitonin (PCT).1,13 Similar to the migraine-like phenotype, COVID-19-specific headache was associated with lymphopenia and high levels of CRP and PCT.13 In contrast, the TTH phenotype tended to be associated with milder forms of COVID-19, characterized by lower levels of CRP and PCT.13
THE PATHOPHYSIOLOGY OF HEADACHE ASSOCIATED WITH COVID-19 MIGHT IMPLY SPECIFIC AND UNSPECIFIC MECHANISMS
In the context of the currently available evidence, researchers have suggested multiple hypotheses explaining the pathophysiology of headache associated with COVID-19. Fever and hypoxia, for example, have been proposed as putative unspecific headache causes—i.e., not related to a direct effect of the virus on the CNS—as they might increase proinflammatory cytokine levels and cerebral vasodilation, respectively.6 Another unspecific mechanism that might lead to headache is the diffuse hyperinflammatory state that the SARS-CoV-2 infection can trigger in some individuals.6 This hyperinflammatory state eventually results in a massive release of cytokines, also known as cytokine storm, which can cause indirect damage to the CNS tissues, thus contributing to the headache onset.6 However, most researchers are trying to unveil specific pathophysiological mechanisms involving the central nervous system (CNS) during and after the SARS-CoV-2 infection, since the presence of viral proteins in the olfactory bulbs, trigeminal branches and trigeminal ganglion suggests that SARS-CoV-2 might reach the CNS,6 cause neuroinflammation and subsequently damage neuronal tissues.12
SARS-Cov-2 might access the CNS via the bloodstream or neuronal retrograde dissemination
The paths by which SARS-CoV-2 accesses the CNS are not clear yet, but two mechanisms have been hypothesized so far: hematogenous spread and neuronal retrograde dissemination.12 According to the first hypothesis, SARS-CoV-2 could infect the endothelial cells of the blood-brain barrier (BBB) or the blood-cerebrospinal fluid (CSF) barrier in the choroid plexus to enter the bloodstream, through which it reaches the CNS.12 Moreover, once in the bloodstream, the virus can also infect leukocytes and exploit them to disseminate across multiple tissues and organs, including the CNS, through a Trojan horse mechanism—12 a strategy by which pathogens hide in circulating body cells, such as leukocytes, in order to gain access to otherwise inaccessible areas. The second hypothesis instead refers to the ability of some viruses to infect peripheral nerves and travel in retrograde fashion to reach the CNS.1 Some authors suggested that SARS-CoV-2 might use its affinity with angiotensin-converting enzyme-2 (ACE2)—a protein expressed on the surface of many cell types, including neurons of the CNS—1 to infect neurons via endocytosis, and then diffuse trans-synaptically to access adjacent neurons.6
THE TRIGEMINOVASCULAR SYSTEM MIGHT BE PIVOTAL IN THE PATHOPHYSIOLOGY OF HEADACHE ASSOCIATED WITH COVID-19
One of the pathophysiological mechanisms that might explain the onset of headache associated with COVID-19 is linked to the activation of the trigeminovascular system (Figure 2).6 Indeed, the nasal mucosa, which is one of the first possible points of contact of the body with SARS-CoV-2,14 is innervated by nociceptive trigeminal afferents.15 The inflammation of the nasal mucosa caused by the SARS-CoV-2 infection may trigger the release of multiple cytokines—such as TNF-α and IL-1β—which activate both the nasal branches of the olfactory nerve and trigeminal nociceptors, and stimulate the release of calcitonin gene-related peptide (CGRP) by the neurons of the trigeminal ganglion.15 The newly released CGRP, in turn, triggers the release of cytokines like IL-1β by satellite glial cells of the trigeminal ganglion, thus initiating a pro-inflammatory vicious cycle.15 Additionally, the activation of the afferent nociceptive fibers in the nasal mucosa triggers the release of CGRP even in the dura mater, to which they extend, thus causing vasodilation and increasing the meningeal blood flow.15 Moreover, in some cases, the strong activation of the mucosal trigeminal nociceptors may lead to a neuroinflammatory cascade that can reach the dura mater and eventually activate meningeal nociceptors, which cause headache.15 This neuroinflammatory cascade might even be further powered by the spinal trigeminal nucleus, which receives inputs from the nasal mucosa and the meninges.15 In some authors’ opinion, the activation of the trigeminovascular system due to COVID-19 —which shows many similarities with migraine pathophysiology—6 might explain the new onset of migraine-like headache attacks in patients affected by COVID-19 who did not have a history of migraine.16 Additionally, the same mechanism might lead to the loss in olfactory function that has been frequently reported by patients during COVID-19.15 Indeed, the high levels of CGRP released by the activated trigeminal system can exert an inhibitory effect on olfactory receptors, thus reducing their response to olfactory stimuli.15
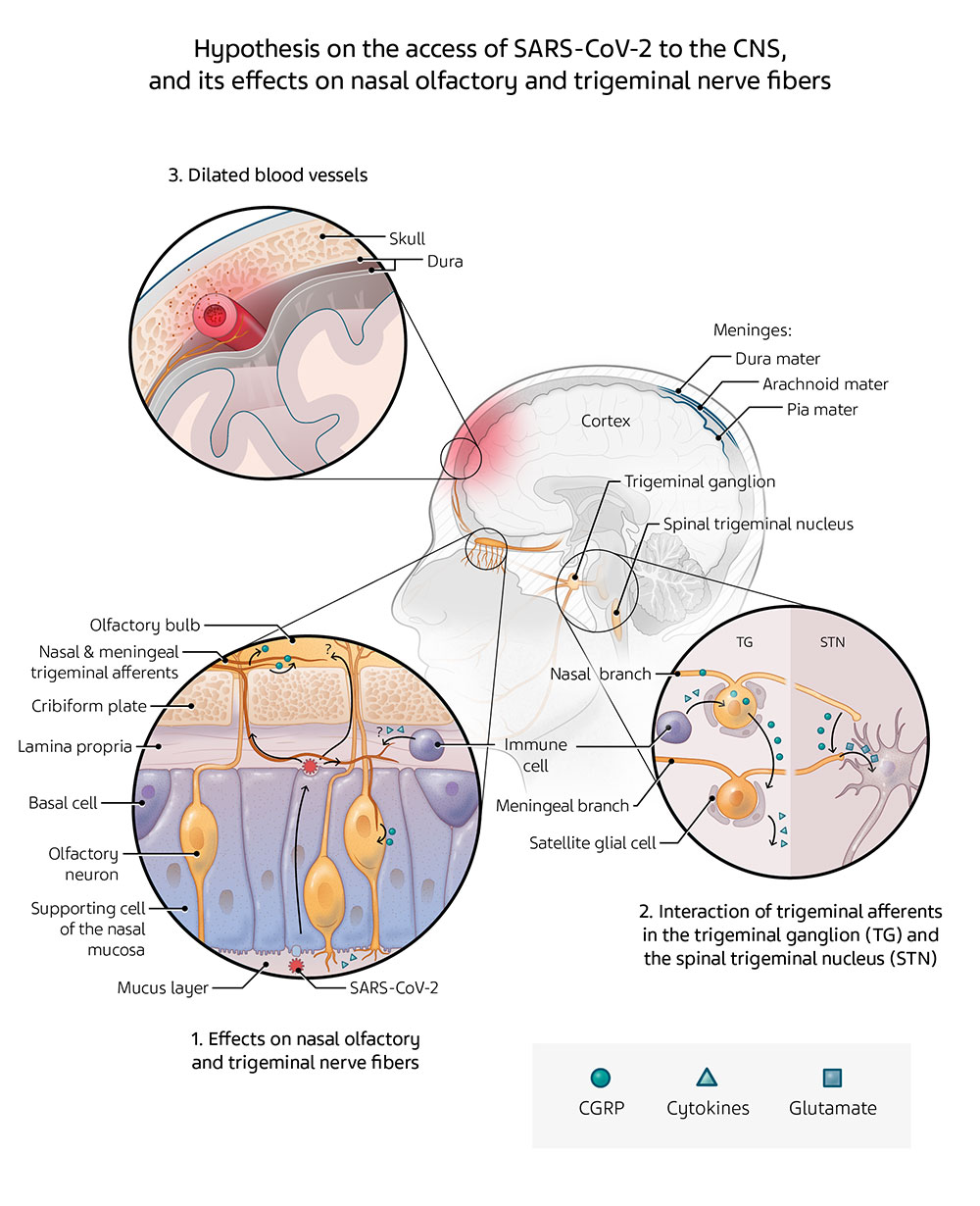
Adapted from Messlinger K, et al. Cephalalgia 2022;42:176-80.
Figure 2. Putative means of access of SARS-CoV-2 to the CNS, and its effects on nasal olfactory and trigeminal nerve fibers
Genetics might explain the increased susceptibility of patients with migraine to headache associated with COVID-19
According to some data, people with a previous history of headache, including migraine, are more prone to experience headache associated with COVID-19.7 For patients with a history of migraine, this susceptibility might be explained by genetic predisposition.1 Indeed, 11 of the 38 genes that have recently been associated with migraine are involved in metal ion homeostasis, thus suggesting a possible link between metal ion imbalance and migraine pathophysiology.1 Interestingly, SARS-CoV-2 showed affinity to zinc, and the subsequent ability to alter its intracellular homeostasis by interfering with the activity of zinc-binding proteins.1 The disrupted zinc homeostasis, along with the genetic susceptibility to metal ion imbalance, might explain why some individuals with a history of migraine are more predisposed to experience migraine-like attacks after a SARS-CoV-2 infection.1
RESEARCH ON COVID-19 AND HEADACHE MIGHT HELP CLARIFY MIGRAINE PATHOPHYSIOLOGY
As COVID-19 continues to be part of our lives, albeit in an ever-evolving scenario, basic and clinical researchers are working relentlessly to gain additional insights on the many aspects of the disease that still need to be clarified. Scientific research on the link between COVID-19 and headache might lead to multiple beneficial results. Indeed, the research studies on the manifold phenotypes of headache associated with COVID-19 could help to elucidate more about the complex pathophysiology of the disease.16 Moreover, they could be a chance to shed light on the unclear details of the pathophysiological mechanisms underlying headache disorders, such as migraine.1
Landis BC, Brooks AE, Digre KB, Seay MD. Coronavirus Disease 2019, Eye Pain, Headache, and Beyond. J Neuroophthalmol 2022. Online ahead of print.
WHO COVID-19 Dashboard. Geneva: World Health Organization, 2020. Available online: https://covid19.who.int/ (last accessed: February 21, 2022).
Crook H, Raza S, Nowell J, Young M, Edison P. Long covid-mechanisms, risk factors, and management. Bmj 2021;374:n1648.
Liguori C, Pierantozzi M, Spanetta M, et al. Subjective neurological symptoms frequently occur in patients with SARS-CoV2 infection. Brain Behav Immun 2020;88:11-6.
Dono F, Consoli S, Evangelista G, et al. New daily persistent headache after SARS-CoV-2 infection: a report of two cases. Neurol Sci 2021;42:3965-8.
Caronna E, Pozo-Rosich P. Headache as a Symptom of COVID-19: Narrative Review of 1-Year Research. Curr Pain Headache Rep 2021;25:73.
Moskatel LS, Smirnoff L. Post COVID Headache: A Case Series from a Tertiary Headache Center”. Poster. Stanford School of Medicine, Palo Alto, CA.
Caronna E, Ballvé A, Llauradó A, et al. Headache: A striking prodromal and persistent symptom, predictive of COVID-19 clinical evolution. Cephalalgia 2020;40:1410-21.
Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497-506.
Borges do Nascimento IJ, Cacic N, Abdulazeem HM, et al. Novel Coronavirus Infection (COVID-19) in Humans: A Scoping Review and Meta-Analysis. J Clin Med 2020;9.
Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int J Antimicrob Agents 2020;55:105924.
Harapan BN, Yoo HJ. Neurological symptoms, manifestations, and complications associated with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease 19 (COVID-19). J Neurol 2021;268:3059-71.
Planchuelo-Gómez Á, Trigo J, de Luis-García R, Guerrero Á L, Porta-Etessam J, García-Azorín D. Deep Phenotyping of Headache in Hospitalized COVID-19 Patients via Principal Component Analysis. Front Neurol 2020;11:583870.
Chavda VP, Vora LK, Pandya AK, Patravale VB. Intranasal vaccines for SARS-CoV-2: From challenges to potential in COVID-19 management. Drug Discov Today 2021;26:2619-36.
Messlinger K, Neuhuber W, May A. Activation of the trigeminal system as a likely target of SARS-CoV-2 may contribute to anosmia in COVID-19. Cephalalgia 2022;42:176-80.
Caronna E, Alpuente A, Torres-Ferrus M, Pozo-Rosich P. Toward a better understanding of persistent headache after mild COVID-19: Three migraine-like yet distinct scenarios. Headache 2021;61:1277-80.